The Good. The Bad. The Ugly. On Prophylactic Bilateral Mastectomy.
I know before my surgery when I was searching (stalking?) every BRCA/prophylactic mastectomy blog out there I could find, I would always scroll to find the posts immediately before and after the blogger’s operation, so I thought I would take the fun out of that and put it all in one place. Assuming you’ve already read how I came to this decision and why, here’s the nitty gritty on the surgery itself.
Timing & Waiting
I purposefully scheduled my surgery super far in advance… like 5 months in advance. I knew I would need to take a few weeks off work, and scheduled my surgery around when that would be best. I needed to have that tangible date… but all the waiting was definitely hard. You can make yourself sick analyzing every detail, but honestly the time just flew by, and I’m so glad I had the time that I did to process everything and get things in order for when I would be gone.
Doctor Decisions: Finding your “Boob Dudes” (or Dudettes)
I think the most important decision in this entire process is deciding who your surgeons are going to be. The surgery is done in two parts – first the breast surgeon comes in and removes all the breast tissue, and then when he’s finished, the plastic surgeon comes in to do whatever reconstruction you have decided on. I am not the best person to talk to about extreme doctor interviewing, because I was so incredibly fortunate to be dropped into the care of two of the most amazing doctors I’ve ever met. My breast surgeon is an internationally recognized BRCA expert, and is the one I initially saw back in 2008 when I received my BRCA results. I went back to him 5 years later, and when we decided to move forward with the surgery, he referred me to “the best plastic surgeon he’s ever worked with.” Which is something to say, when you’ve been doing this for 17 years! I was beyond impressed when I met said plastic surgeon 3 days later, so I had no need to seek a second opinion. My advice, however, is to make sure that your surgeons work together on a routine basis, and that you can put your trust in them one hundred percent. Because that’s exactly what you’re going to do.
Procedure Options
“Options” is an understatement because WOW want to talk about a mouthful of alphabet soup?? Do a little research on breast reconstruction! Basically you have two major options: autologous (flap) surgeries where your own tissue is used to reconstruct breasts, or implant reconstruction. Because of my age and body, I chose implant reconstruction, specifically immediate reconstruction with tissue expanders. There is a decent possibility that I will consider a flap surgery later on, as implants don’t last forever, and my plastic surgeon definitely presented it as an option for later, particularly after having kids. But for now, implants are the way to go for me.
I did consider “direct to implant” reconstruction, where you actually get your permanent implants put in all at the same time. To me, the biggest pro was obvious: get it all done at once. And originally I was so focused on getting rid of my risk that I was going to stay the same size and just be done with it. However, the more I researched it and talked to other people my age, and then of course my breast and plastic surgeon, I quickly realized that expanders were the way to go for me. From my breast surgeon’s perspective, he did not want any additional stress on my tissue and skin, but just for the skin to “lay” over the expanders. That totally made sense. And then from my plastic surgeon’s perspective, he wants me to have a part in the process, particularly in deciding size. I also came around to realize that if I’m going to have to go through this crappy surgery, I might as well make the best of it and get bigger, beautiful boobs out of it! No I’m not going crazy, but I am going a little bit bigger to better fit my shoulders and build.
The con of expander reconstruction is, of course, that there is an additional surgery. A few weeks after the original surgery where the expanders are placed, you begin getting “fills.” The expanders have a metal port on them that can be found with a magnet, and a needle placed and saline is injected, little by little, every few weeks. Then you have an “exchange surgery,” this happens a few months after the original mastectomy surgery, when the expanders have been filled with saline as large as they will be. However, it’s very short, outpatient, and the recovery is much less than the first surgery. This really wasn’t a big deal to me, if it would get me the best result.
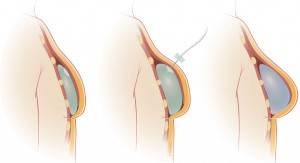
Illustrated, this is what the expander process looks like: on the far left, the expander is placed under the muscle immediately after the mastectomy. In the middle, the needle injecting saline into the port to fill and expand, slowly stretching the muscle. And on the right, after the exchange, the final implant is placed.
Nipple Sparing or Not?
I chose to have a nipple-sparing procedure. My surgeons do them ALL the time, so I really didn’t feel like I was taking a risk, particularly when the latest research has shown that NSM (nipple-sparing mastectomy) is safe, even in BRCA carriers. It was important to me, at the age of 25, to keep my nipples to get the most natural result possible. Don’t get me wrong, the things they can do with nipple reconstruction are simply amazing. And if we had a history of cancer in the nipple, or if I wasn’t a good candidate, I definitely wouldn’t have done it. But thankfully I’ve always said no to cocaine and smoking (no seriously! Those are big risk factors for losing blood supply!) Not all surgeons do this routinely, but after seeing the results my surgeons have had, it was an easy decision, and one I’m glad I made.
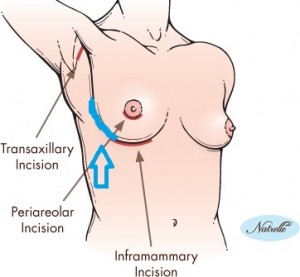
The other big consideration with this was the location of incisions. With nipple-sparing, my surgeons were able to use inframammary fold incisions. As you can see below (ignore my absolutely terrible Paint skills – I know I fail as a child of the 90s!), they’re SO easily hidden – I hesitate to even use the traditional “inframmary fold” explanation for mine because they are so far on the sides, so I drew my own in the turquoise. In head-on pictures, you honestly can’t see them. Amazing? I think yes.
Sentinel Lymph Nodes?
I had a completely clean MRI in March before my surgery, so no one expected to find anything cancerous (and thankfully, this was correct, with a completely benign pathology report that I received from my breast surgeon on Friday after my surgery). However, I truly appreciate how cautious my breast surgeon is, and how seriously he takes reducing my risk as much as possible, so I did have sentinel node biopsies done during the first part of my surgery. This means that he took 2 axillary lymph nodes from each side, and sent them to pathology while I was under, to make sure there were no questionable cells. It adds a little bit of time to the surgery, but is so worth it in my opinion. I can’t imagine having to go BACK to the OR if they found something later in pathology. All this added to the process from my end was having lymphoscintigraphy done the day before after I met with the pre-op nurse and had labs drawn. Basically they injected a radioactive isotope into each areola (really not as bad as it sounds!!) and then I came back 2 hours later for a scan to identify the nodes. And then got to go home with radioactive boobs. Not a difficult process at all, and totally worth it for the additional peace of mind!
The D-Day Deets
The Big Day was on Tuesday, August 6, 2013. I had to arrive at the hospital at 10 am, and things just kept moving from there! I was so blessed to have both of my parents, and 3 of my best friends (roommate, WorkFave, and of course Ruthie – who was there from the beginning) there that morning – and trust me, that was at their insistence! But I love them for it. I took one last pre-op selfie, and dawned my lovely gown, thigh-high TED hose, and gripper socks. What can I say, I was bringing sexy back. And they were all coming with me.
I had a great pre-op nurse who was totally on the ball. Consents were reviewed and signed. My plastic surgeon, Dr. Teotia, was in right away to draw all over with a number of colored sharpies. My breast surgeon, Dr. Euhus, was in soon after, and we went over all the last minute details. My anesthesiologist and CRNA were totally BA. I felt so well taken care of – we were all calm, which came from within, as we all knew this was the right decision and I honestly don’t think I could have been more prepared.
I texted the 3 girls, who were by then out in the waiting room, at 12:34 pm that “We’re off!! Love you all thank you so much for being here and keeping mom company!” as my parents kissed me goodbye see you later. I was given some “IV margarita” and we were off to the OR. The last thing I remember was sitting up to help the CRNA get EKG electrodes on my back, and then it was nap time!
Mom posted on Facebook at 6:11 pm “Diana is now in recovery. Both surgeons said everything went very well.” Actually it should have been more like all THREE surgeons said everything went very well. Yeah about that… Despite the title of this post, here I describe my VP shunt that goes from my brain to my abdomen that I’ve had since 2006. At pre-op with my breast surgeon, we discovered, from my MRI in March, that it actually went right through my breast tissue. What can I say, I wanted to keep them on their toes! Actually this was a big concern, and rightly so. I actually kind of expected something to happen, call it intuition or my own genuine appreciation for being a shit magnet (my own mother admits this), so I wasn’t surprised to hear that it got in the way and my neurosurgeon had to come in and fix it. But it was an easy fix, and it actually is a relief to me to know that my breast surgeon is THAT thorough in getting out all the evil cancer-making breast tissue. And honestly if they hadn’t told me, I would have never known anything happened – that’s how awesome they all are! Thankfully we were very cautious in advance, and my neurosurgeon was right there to fix it. So anyhow, after almost 6 hours in the OR I was moved to the PACU.
I have vague memories of waking up and getting pain/nausea medicine and a chest x-ray (to check my shunt placement), but I do remember talking to both of the Boob Dudes. In particular, my plastic surgeon, because he was thrilled to tell me that he placed 600 cc expanders bilaterally (along with Alloderm) and was able to fill 500 cc in EACH expander!! That was such awesome news, meaning I’d only need 2-3 fills total, and that I never really felt that I lost anything. They removed 560 grams of tissue from my right breast and 470 grams from the left. So take the average, and I woke up with almost exactly what I started! Seriously. Modern medicine astounds me.
I really was feeling pretty darn good by the time my Mom posted, at 7:57 pm, that I was “Out of recovery and in her room. Everything went well.” Here I am rolling into the room, with my parents and 3 of my best friends (one had been swapped out!) waiting for me:
The Hospital Recovery
My whole time in the hospital is a little bit of a blur now, but I felt much more lucid at the time, and really couldn’t have asked for a better experience. While it was kind of weird not having my surgery be at the crack of dawn, it ended up being fantastic timing. Since I didn’t get up to my room until 8, we were able to metaphorically ‘coast through’ the first night. I had a Foley catheter so I didn’t have to get up to pee, which was such a good thing – I seriously don’t think I moved my arms the entire first night. And I had my morphine PCA button. That was really all I needed! Haha. My PACU nurse was on top of it and ordered me some food before it was too late, which was waiting for me when I got up to my room. Dad definitely had to “airplane” feed me mashed potatoes. That was really the only time I had that raw, fresh post-op pain, and I think I was more scared to move than anything!
I was in a swanky black mastectomy bra for the first 48 hours that really kept the swelling down, and everything in place. I also had 4 JP drains, 2 on each side. I didn’t think they were as terrible as everyone described, but it was a HUGE relief to get them out (2 at post-op day 9, the remaining 2 at post-op day 16). These are what the bad boys look like – the insertion site covered (yes I bruise like a peach), the insertion site a couple days before the last ones were pulled – note the hole to the right from the previously pulled drain, and the bulbs collecting the lovely “boob goo”:
I was also in a clinical trial for a special dressing that is supposed to help with blood flow and healing in nipple-sparing mastectomy. That was on my right side, and was changed daily for a week, while my left side was the “control” side. Overall my nipples survived very well, minus a bit of pigment loss, which was expected and is totally fixable.
I was in the hospital for a total of 2 nights. The next morning I had my Foley pulled, was started on oral pain meds (which they had scheduled so I didn’t have to ask for them, which was great), and was able to get up and move around. It was obviously painful at first, but putting on real clothes and brushing my teeth made a huge difference:
I struggled with some nausea but we got it under control by the afternoon with some Phenergan (I already had Zofran). I had a bunch of lovely visitors that kept me entertained, as well as the guest services people bringing me DVDs to stay distracted – Legally Blonde, Meet the Parents, and Mona Lisa Smile did an excellent job of that! My biggest struggle that day, and really of the entire process, were with muscle spasms. The best way I can describe it is to imagine your entire breast being grabbed and twisted, like a Charlie Horse that you can’t stretch out. They got much better after my first set of drains was pulled (they were irritating the muscle more than I realized!), and Flexeril, a muscle relaxer, helped as well.
As for pain medicine, I was on hydrocodone 10/325 for one week after surgery – I started halving the doses after about 5 days, and then switched to plain Tylenol. That, along with the Flexeril, worked very well, and I was so thankful to not have to deal with withdrawal symptoms that I read horror stories about. I took it around the clock, including throughout the night, for the first few days, so that time is a big giant blur, but I’m okay with that. Other meds I was on: Colace (which didn’t help a whole lot… I added Miralax and finally took Mag Citrate when I got frustrated 4 days later), and Keflex. I actually ended up having 2 weeks of Keflex, since my drains were still in plus the shunt and a small open area of my right nipple, so my plastic surgeon was cautious.
My night nurse in particular was fantastic, and the second night I actually got some decent sleep. The next morning I saw both my surgeons, and we were “bustin’ out of there” by noon.
The Extended Recovery
I took it really easy at home for the first week – the recovery wasn’t all rainbows and butterflies, and I won’t sugar coat to say that it was. In fact, I didn’t leave the house until my one-week post-op visit with the plastic surgeon the following Thursday. I watched lots of DVDs and slept a TON. My parents were incredible and waited on me hand and foot – even though my range of motion was really pretty good, it was so important not to overdo it with moving and lifting. I had those first 2 drains (#1 and 4) pulled that day, and finally the stir crazy started to set in. I made it out to the grocery store the following day, and my recovery really picked up from there. By two weeks out, I was really doing pretty well. My biggest struggles were sleep (it’s just really difficult to get comfortable with expanders and drains), muscle spasms (though they were decreasing), and nerve pain. Nerves are NOT impressed with being cut!! But that is an unfortunate necessity of the surgery. It’s like a prickly burning all around my torso – very weird, indeed.
It was at my second post-op visit, when I had my remaining drains pulled and my first expander fill, that I really turned the corner, so to speak. Can you imagine I felt better after THIS was out?
I also had my first expander fill that day (50 cc on each side), and I was cleared to drive and increase my activity, which made a huge difference – I felt “free” and was able to slowly increase my independence again. I followed up with my breast surgeon the following Monday, and moved back to my apartment the same day. I took it easy there for a couple days, and was back at work just 3 weeks after I was discharged from the hospital.
One week after that (two weeks from my last plastic surgery appointment), on September 5th, I saw Dr. Teotia again, and had my second and final fill of 50 cc’s on each side, bringing the total to 600 cc filled in each expander. I also got to schedule my exchange surgery!! This was so exciting, and just a little bit crazy. I had a total of 3.5 months with expanders, which really went by pretty quickly. But by the time it came around, I sure was ready to evict those turtle shells!!
The Exchange
My exchange surgery was on November 22nd, strategically scheduled for the Friday before Thanksgiving, which minimized how much work I would miss. It was by far the most seamless surgery experience ever! I totally had the “A Team” that day – on top, my surgeon, Dr. Teotia (on the far right) and the rest of the team in the OR, Ruthie and I with Dr. T in pre-op, and me giving a slightly Versed-accentuated thumbs up of how excited I was to be at that point!!
Unlike the mastectomy, this was day surgery and took just a couple of hours for the actual procedure. My previous incisions on the sides of my breasts were reopened, expanders removed, and final implants placed. My plastic surgeon and I had agreed on 640 cc Natrelle 410, moderate height, full projection implants – aka tear drop “gummy bears” – given that nickname, because you can slice through the silicone and it doesn’t leak. So far, I am absolutely loving them, and so impressed with how natural they look. They are much like my real breasts, just fuller with better shape and projection. In addition, he reinforced my left side that liked to rotate laterally with Strattice (pig skin), which fixed the problem, and I had fat grafting done at the same time – I’m SO glad I did it all together! My surgeon took fat (using liposuction) from right below my breasts, my outer thighs, and flank area, and injected it above and to the sides of the implants, to give a better slope – I had a lot of breast tissue up high (that was removed in the first surgery), so this helped immensely to make them look great without crevices or gaps.
As for the recovery, I was honestly more sore from the fat grafting than from the expander/implant exchange! The bruising was impressive and I had to wear compression leggings/garments for a good two weeks, and was still sore, but it was so worth it. I took pain medicine for a couple days and took it easy for about a week and a half, but still a much easier recovery than the mastectomy – did I mention no drains?! Also, the relief of being DONE helps the recovery immensely! 🙂 I followed up with my plastic surgeon two weeks later where they took out stitches and removed all the tape, and simply made sure everything looked good, which thankfully it did – great even!
The Future
Writing a few weeks after my final surgery, I’m in the final follow-up phases and doing remarkably well overall. Thrilled to be done with the surgeries, and enjoying the relief that came with them. It’s been quite the almost year-long journey, but totally worth it. Now all ahead of me is perhaps some finishing touches, and routine follow-ups with my plastic and breast surgeons.
I was often asked if I had doubts, or second thoughts, leading up to my surgery or immediately after. I am thankful that I can confidently answer “no!” I had done my research, talked to the experts for the medical side of things, talked to my family and friends for the emotional side of things, and had plenty of 3 am thought-sessions with myself to know that I was making the right decision. The relief I felt when I woke up, and knew I had taken my risk of breast cancer from 87% to less than 10% in six short hours, is truly indescribable. With reconstruction as amazing as it is, I never woke up flat, and truly don’t feel like I “lost” anything – all I did was gain empowerment. I am so grateful to be given the gift of knowledge, so that I could do something about it. And I’m so glad that I did!